For Patients
Cervical cancer
Introduction
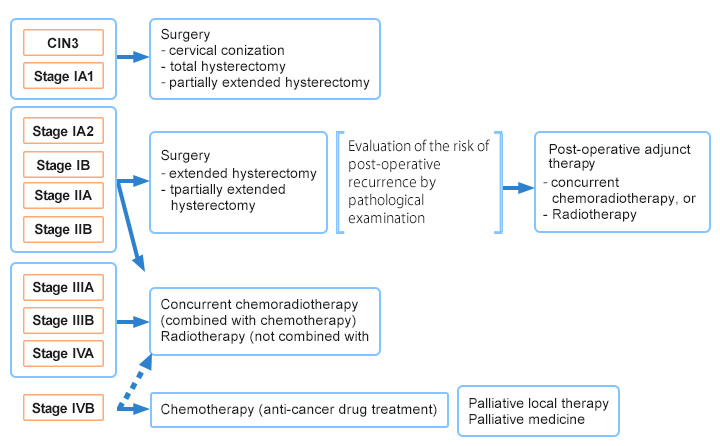
Cervical cancer is a malignant tumor mainly caused by the infection of the cervix with human papillomavirus (HPV), and is the second most common disease in female reproductive organs after uterine body cancer. Histologically, squamous cancer accounts for approximately 75% and adenocarcinoma about 23%, with the proportion of adenocarcinoma increasing every year. It is characterized by being common among grand multipara and young women, and is the second most common invasive cancer in women aged 25-34 years after breast cancer. The peak age of its onset is in the 30s to 40s, but advanced cancer has been reported to increase after the 60s (Fig. 1).
Figure 1 Age distribution of cervical cancer by advancement stage
Report from the Gynecologic Oncology Committee of the Japan Society of Obstetrics and Gynecology, 2017 Annual Patient Report
(Acta Obstetrica et Gynaecologica Japonica (2019) 71, 686)
Symptoms
Cervical cancer is known to become cancerous through a precancerous condition called dysplasia (cervical intraepithelial lesion), which can be detected by a cytological examination before it advances to cancer.
Usually, there is no subjective symptoms at the time of precancerous condition or the beginning of invasion, besides contact bleeding associated with sexual contacts. Therefore, having medical examinations from asymptomatic stages is important.
Once the cancer advances, low back pains due to hydronephrosis and hematuria/hematochezia sometimes occur due to the invasion into the bladder/rectum.
Screening
Cancer screening usually involves only cytodiagnosis. When any abnormality is suspected by cytodiagnosis, a histological examination and a colposcopic examination (vaginal magnifying glass test) are performed for thorough examination. In addition, pelvic examination, ultrasonography, as well as CT and MRI examinations are used to examine the spread of cancer.
<Cytodiagnosis>
Cells around the opening of the uterus into the vagina (external uterine orifice) are collected by rubbing this area with an apparatus to check for abnormal shape of cells. All the results obtained by cytodiagnosis are "suspicious diagnoses," and cytodiagnosis alone does not provide definitive diagnoses.
<Tissue diagnosis>
When any abnormality is found during cytodiagnosis, small pieces of tissue are cut from the suspicious site and diagnosed under a microscope. This test is used to make a definitive diagnosis of cervical cancer.
<Colposcopic examination>
Mucosal surface of the cervix is magnified to observe small parts using a magnifying glass called colposcope. The diagnostic accuracy of tissue diagnosis is considered to improve by collecting the tissue from the site where abnormality was suspected in colposcope observation.
<CT/MRI examination>
CT scan uses X-rays and MRI scan magnetism for depicting the inside of body to check for possible metastases and the invasion of cancers to surrounding organs before treatment. Usually, MRI scan can depict cervical lesions more clearly. Therefore, MRI examination is used for the scrutiny of pelvic lesions. Meanwhile, CT examination is used for the diagnosis of metastasis to distant organs such as the lung and the liver as well as lymph node metastasis, as it allows simultaneous examination of wide areas.
Clinical stages
The term "stage of advancement" refers to the degree of cancer progression. Classification of the stage is based on the depth of cancer invasion into the mucosa and the presence of metastases to distant organs such as the lung as well as lymph node metastases, besides the size of cancer (Table 1). Five-year survival rate for each stage of cervical cancer has been reported as shown in Figure 2.
Table 1. Classification of cervical cancer by clinical stages (Acta Obstetrica et Gynaecologica Japonica (2011) FIGO2008)
| Stage I | Cancer is found only in the cervix and has not spread elsewhere | |||
|---|---|---|---|---|
| Stage IA | Invasive cancers that can be diagnosed only histologically, with the depths of stromal invasion of 5 mm or less and vertical spread of 7 mm or less. | |||
| Stage IA1 | Invasive cancers that can be diagnosed only histologically, with the depths of stromal invasion of 3 mm or less and vertical spread of 7 mm or less. | |||
| Stage IA2 | Invasive cancers with the depths of stromal invasion of 5 mm or less but exceeding 3 mm with vertical spread of 7 mm or less. | |||
| Stage IB | Clinically obvious lesions localized to the cervix | |||
| Stage IB1 | The sizes of lesions are 4 cm or less | |||
| Stage IB2 | The sizes of lesions exceed 4 cm | |||
| Stage II | Cancers spread beyond the cervix but have not reached the lower third of the pelvic or vaginal walls | |||
| Stage IIA | Cancers have spread to the vaginal wall but not to the tissues surrounding the cervix | |||
| Stage IIA1 | The sizes of lesions are 4 cm or less | |||
| Stage IIA2 | The sizes of lesions exceed 4 cm | |||
| Stage IIB | Cancers have spread to the tissues surrounding the cervix but have not reached the pelvic wall | |||
| Stage III | Cancers have reached the pelvic wall without non-cancerous part between the cancers and the pelvic wall, or their invasion to vaginal walls have reached their lower 1/3. | |||
| Stage IIIA | Cancers have spread to lower 1/3 of the vaginal wall, but the spreads to the tissues surrounding the cervix have not reached the pelvic wall | |||
| Stage IIIB | The spreads of cancers to the tissues surrounding the cervix have reached the pelvic wall, or the ureter that connects the kidney to the bladder has been crushed by cancer, resulting in hydronephrosis or nonfunctional kidney | |||
| Stage IV | Cancers have spread beyond the small pelvic cavity or to the mucosa of the bladder and the rectum | |||
| Stage IVA | Cancers have spread to the mucosa of the bladder and the rectum | |||
| Stage IVB | Cancer metastases have occurred beyond the small pelvic cavity | |||
Figure 2. Five-year survival rate by the stages of cervical cancer for the cases diagnosed in 2012.

Report from the Gynecologic Oncology Committee of the Japan Society of Obstetrics and Gynecology, the 60th Annual Treatment Report
(Acta Obstetrica et Gynaecologica Japonica (2019) 71, 738)
Treatments
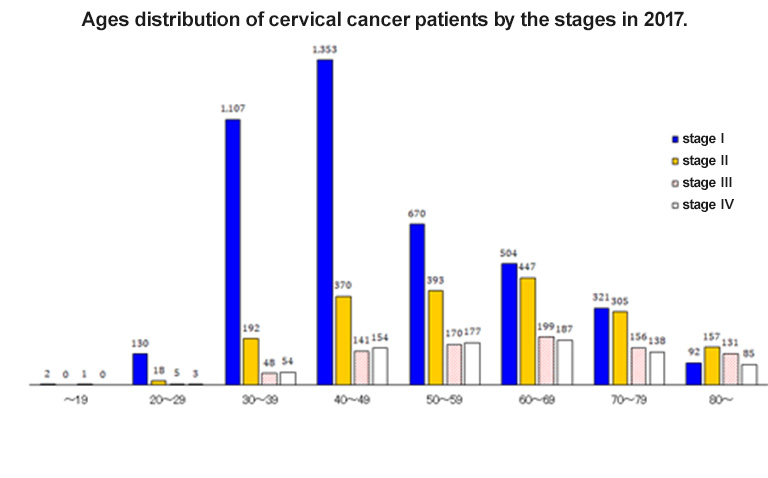
Treatments of cervical cancer include surgery, radiation therapy, and chemotherapy (treatments with anticancer drugs). The choice of treatment is made based on the conditions such as cancer stages, age, and the presence of complications (Fig. 3).
Fig. 3. Clinical stages of cervical cancer progression and approaches for treatment